
Today, we commemorate World NTD Day for the fourth time. In this article, I look back over the past 25 years and highlight key developments that have brought neglected tropical diseases (NTDs) out of the shadows and into the forefront of global health. And I look ahead in the spirit of this year’s theme: “Unite. Act. Eliminate”.
Concerted Efforts to Tackle Poverty-Related Diseases
Momentum picked up in the year 2000, with the launch of the United Nations Millennium Development Goals (MDGs). With a target date of 2015, the MDGs provided a blueprint agreed on by all countries and leading development institutions to tackle poverty, hunger and ill-health. Three of the eight MDGs were health-related, focusing on child and maternal health as well as on combatting “HIV/AIDS, malaria, and other diseases”.
The MDG era spurred an unprecedented global health effort, facilitated by a steep increase in funding for research and development (R&D), a significant increase in development assistance for health, the establishment of the Global Fund, and the creation of product development partnerships (PDPs), such as Medicines for Malaria Venture (MMV), FIND and Drugs for Neglected Diseases initiative (DNDi).
The Birth of the Term “Neglected Tropical Diseases”
The term “neglected tropical diseases” was officially coined in 2005, thanks to the publication of a couple of seminal papers. These peer-reviewed publications underscored the social, economic and public health importance of a diverse group of poverty-related diseases. The authors emphasised that the collective burden of an initial group of 13 to 15 NTDs was similar to that of any of the ‘big three’ killer diseases HIV/AIDS, malaria and tuberculosis.
As an external reviewer of the Hotez et al. paper in PLoS Medicine, I anticipated that its publication will mark a turning point in raising awareness of the NTDs, including the epidemiology, prevention, diagnosis, integrated control and elimination. Indeed, forces united and research in the fight against NTDs intensified. In October 2007, PLoS Neglected Tropical Diseases was launched as the first open-access, peer-reviewed journal entirely devoted to the NTDs. Since then, this journal has established itself as the flagship outlet for research in this field with more than 10,000 articles published thus far.

Officialising NTDs brought about action: On 30 January 2012, endemic countries, donors, pharmaceutical companies and non-governmental organisations (NGOs) came together to sign the London Declaration on Neglected Tropical Diseases. Together, they pledged to control, eliminate or eradicate 10 diseases by 2020 and improve the lives of more than a billion people.
Today, the World Health Organization (WHO) lists 21 NTDs, such as Buruli ulcer, Chagas disease, food-borne trematodiasis, human African trypanosomiasis, leprosy, rabies, schistosomiasis and soil-transmitted helminthiasis. All of these diseases occur primarily in among impoverished communities in tropical and subtropical areas, perpetuating a cycle of poor educational outcomes and missed employment opportunities, and are associated with neglect, social exclusion and stigma.
From Silos to Synergies
The recognition of NTDs led to a shift from isolated efforts to collaborative approaches. Innovation, R&D and control/elimination efforts were diversified across diseases. Pharmaceutical companies played a key role by donating the few available drugs with proven efficacy and safety. The public and private sectors also teamed up to fill the empty treatment pipelines. The Pediatric Praziquantel Consortia, for example, brought together Merck, Astellas, Lygature, Swiss TPH and others to develop a new formulation of praziquantel for the treatment of schistosomiasis in preschool-aged children. In the HAT-r-ACC consortium, Swiss TPH joined Sanofi, DNDi and other partners to develop fexinidazole as a new treatment for human African trypanosomiasis (HAT).

From Science to Impact
Both consortia reached major milestones at the end of 2023 when the European Medicines Agency’s (EMA) adopted a positive opinion for arpraziquantel for the treatment of schistosomiasis in children aged three months to six years and a positive opinion for fexinidazole as the first oral treatment for Trypanosoma brucei rhodesiense, an acute form of HAT.
Of course, the availability of drugs is not enough to sustainably control and eliminate NTDs. Beyond medical interventions, we need a deeper understanding of the social-ecological contexts and health systems in disease-endemic regions. By taking a holistic approach, we can ensure that medicines and other essential tools reach those who need them most, tailor interventions to local needs, empower communities in endemic settings and strengthen health systems to break cycles of transmission.
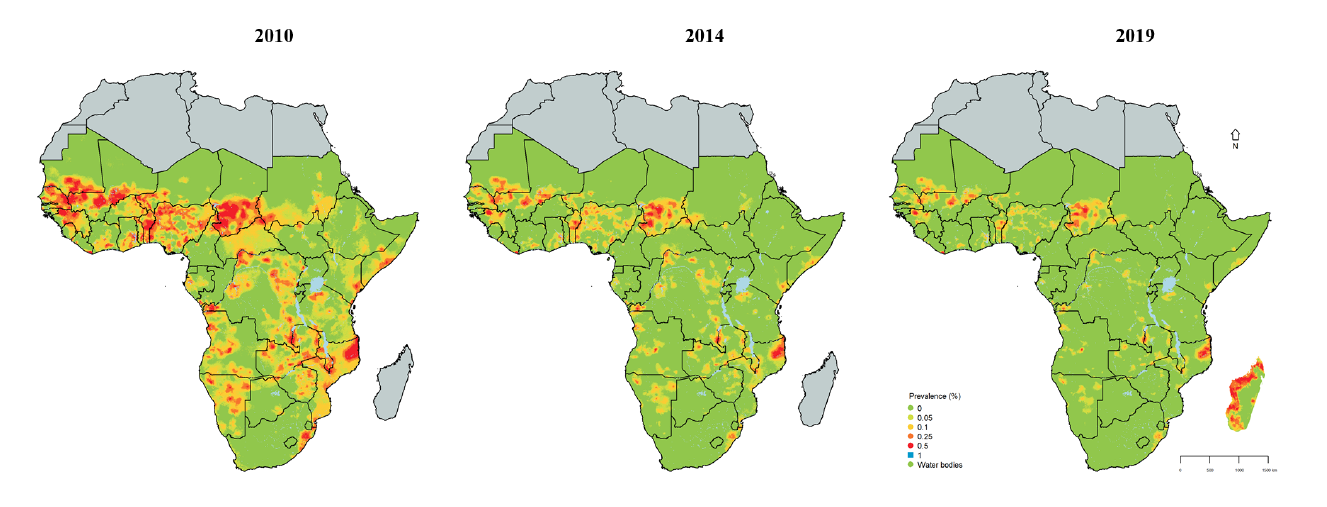
A great example of where joint efforts led to measurable impact is in the area of schistosomiasis, a parasitic worm infection affecting an estimated 250 million people worldwide. Pursuing a spatio-temporal analysis with advanced Bayesian geostatistical modelling, Swiss TPH and partners were able to show that the risk of Schistosoma infection in sub-Saharan Africa over the past 15 years was reduced by more than 60%.
Towards A World Where No Disease Is Neglected
We have come a long way in the fight against NTDs over the past 25 years. But on today’s World NTD Day, let us not rest on our laurels but rather look forward to address the challenges ahead:
- More and better drugs, diagnostics and vaccines are still needed to combat many of the NTDs, such as chikungunya, dengue, leishmaniasis and soil-transmitted helminthiasis, to name just a few.
- Surveillance, control and elimination efforts need to be enhanced to detect patients affected by stigmatising diseases, such as Buruli ulcer, leprosy and noma.
- Intersectoral collaboration and health systems need to be strengthened to tackle zoonotic NTDs, such as food-borne trematodiasis, rabies or schistosomiasis.

And let us not forget about those diseases that are so neglected that they are not even recognised as such! I commend WHO for keeping the NTD list dynamic and for instance adding the debilitating orofacial disease noma in December 2023. Only through awareness can we create knowledge and only through knowledge can we tackle an issue appropriately.
Therefore: let us unite and act together towards a world where no disease is neglected and where no patient is left behind. The tasks ahead are formidable, but together, we can end the neglect and control and eliminate NTDs for good.