Making the world a healthier place
Excellence in Science

We discover novel diagnostics, drugs and vaccines and develop new approaches and tools.
Taking Science to Impact

We integrate new treatments and approaches into policy and health systems.
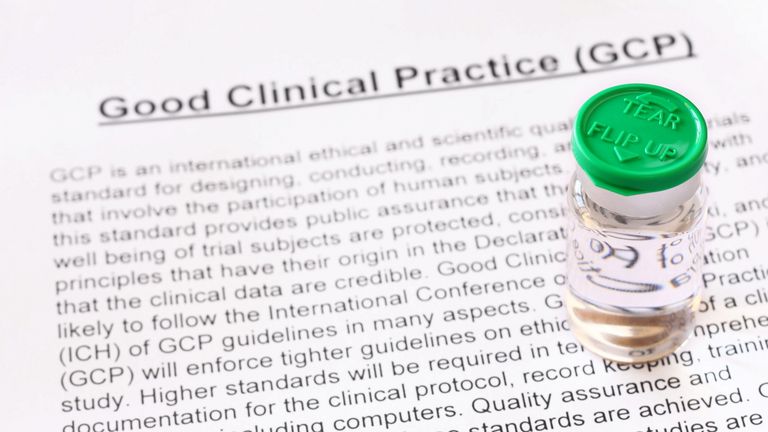
Mutual Learning

We offer local and international training programmes and courses at graduate and postgraduate levels.
Improving Health Worldwide
Swiss TPH is a world-leading institute in global health with a particular focus on low- and middle-income countries. Around 1,000 staff and students from 96 nations work at Swiss TPH focusing on climate and environment, infectious and non-communicable diseases, societal and cultural context, and health systems and policies. We are dedicated to improving the health and well-being of people – locally, nationally and internationally – through excellence in research, education and services.